A research division at HealthPartners has received $2 million from the federal government to monitor the safety of new COVID-19 vaccines for pregnant women and their babies.
For months, obstetricians have pushed to make sure access to the new vaccines isn't denied to pregnant and postpartum women, a group that includes an estimated 300,000 health care workers who are among the first to be eligible.
Federal guidance says pregnant women in groups with priority can choose whether to get vaccinated, and suggests that they can talk with their doctors about risks and benefits. Since large clinical trials of the vaccines didn't include pregnant women, the new studies are designed to help fill information gaps about whether there are pregnancy-specific risks, said Dr. Elyse Kharbanda, a researcher at the HealthPartners Institute.
"All data suggests that the vaccines should be safe — we don't have evidence of any specific risks," Kharbanda said. "It's just that we need to do these studies in order to have the evidence."
She added: "I think many obstetricians are following [professional] guidelines — telling women that the vaccine shouldn't be withheld, and they should have access to the vaccine. But that doesn't always help an individual trying to make this decision during their own pregnancy."
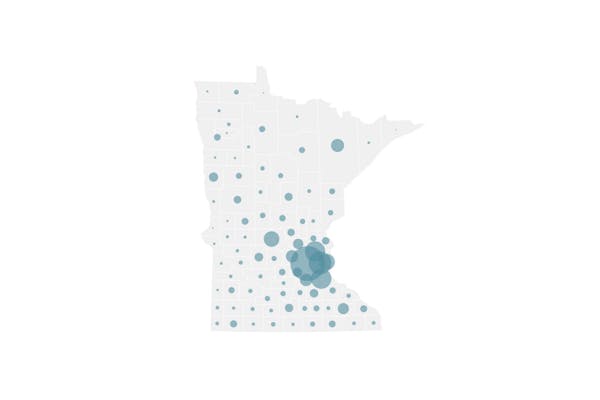
The federal Centers for Disease Control and Prevention is funding the research. HealthPartners and eight other large health systems already have worked to monitor the safety of several other vaccines in use across the United States.
With the COVID-19 vaccine, the HealthPartners Institute will jointly lead the project with a researcher at Yale University.
Two vaccines against the pandemic coronavirus are being used in the United States under an emergency use authorization. Currently, the United Kingdom is not routinely recommending vaccinations for pregnant women, but doctors in the United States have argued women should weigh risks and benefits for themselves, said Dr. Mark Turrentine, a physician who helped develop vaccine guidance for patients for the American College of Obstetrics and Gynecology.
"Symptomatic pregnant women with COVID-19 are at an increased risk for more severe illness compared to their nonpregnant peers, although the absolute risk is low," Turrentine said. "So, definitely there is a rationale for offering a potential vaccine."
Limited studies in animals have not shown any alarming signals from the vaccines for offspring, Turrentine said. The vaccines don't use live viruses, he added, nor do they alter a recipient's DNA or have ingredients that are known to be harmful.
But doctors counseling patients must explain that there aren't studies that show how well the vaccine will work in pregnant women, Turrentine said, or if there are unique downsides. He noted that even with seasonal flu, where the safety profile of vaccines is well established, at least 40% of pregnant women opt for vaccination.
With COVID-19, doctors can't yet quantify how much more risk pregnant women face from the disease, Kharbanda said. At the same time, any risks of vaccination are theoretical.
"It's a difficult situation for pregnant women when making these decisions," Kharbanda said.
Individual factors are key, doctors say, such as whether a pregnant woman can work from home or otherwise minimize potential virus exposure. Patients also will consider if they have health problems that put them at greater risk from COVID-19.
While the decision might pose "somewhat of a dilemma" for some women, obstetrician Margaret Sweeney said she opted to be vaccinated even as she's breast-feeding her 5-month-old son. Because she's regularly seeing clinic patients, some of whom have COVID-19, Sweeney thought the vaccine would help reduce any risk of bringing home the virus to her baby and grandparents helping with child care.
Sweeney said a number of pregnant and lactating health care workers she knows have opted for the vaccine.
"The vaccine has not been directly tested on pregnant women," Sweeney said. But, in general, studies have shown few side effects, she said, adding that it "really has low theoretical risk of causing any complications or harm for pregnancy."
Dr. Justine Trumm, a family physician at M Health Fairview, said she plans on getting the vaccine but will wait until after she delivers her baby. The decision isn't based on concerns about the vaccine, she said, but is more about timeline — since she's already in the third trimester of her pregnancy, she's opting to control potential exposure through personal protective equipment at work.
Doctors face somewhat of a challenge in counseling patients due to the lack of data about the vaccines in pregnant women, Trumm said, but she called it a "great benefit" that pregnant and lactating women have the option.
"As we're learning more and more about COVID-19, there are certainly risks for pregnant women that seem to be higher than for the general population," she said. "So, it's important for us to be thinking about vaccinations in this population, even though we don't have as much data or all the information that we would prefer to have."
At HealthPartners, the five-year study will evaluate data from participating health systems to understand the risk of adverse pregnancy and birth outcomes following COVID-19 vaccination. It also will assess if vaccines impact infant development. A second three-year study will look at whether there are risks of stillbirth and miscarriage following COVID-19 vaccination in pregnant women.
"Vaccines will be the best way to overcome this pandemic, and these projects are part of the process of ensuring the vaccines in use are effective and safe," Kharbanda said in a statement.
Christopher Snowbeck • 612-673-4744
Twitter: @chrissnowbeck
Two teens wounded, one seriously, in north Minneapolis shooting

How did gambling develop into a major industry in Minnesota?
Myon Burrell arrested on probable cause of narcotics violation
Brooklyn Park community development director departs for Bloomington