The Minnesota Department of Health is going door to door across the state to find volunteers for free COVID-19 diagnostic and antibody testing to assess the actual spread of the pandemic.
While Minnesota as of Tuesday had reported 1,927 COVID-19 deaths and 85,351 infections with the novel coronavirus that causes the disease, that doesn't include thousands of people who suffered mild or asymptomatic cases and never sought testing.
State health officials said an accurate assessment is needed to inform Minnesota's pandemic response and to identify hot spots at risk for more cases. Prevalence studies also indicate if the population is getting closer to a level of "herd immunity" that chokes the spread of the virus.
"With a new virus, we have to learn as we go and adapt our response based on new data," said Dr. Ruth Lynfield, state epidemiologist. "Information we gather in this survey will allow us to refine our recommendations to best meet the needs of our Minnesota communities in the prevention of COVID-19."
COVID-19 survey team workers will offer in-person testing this month to households in 180 neighborhoods, which were selected across Minnesota to generate a random but diverse group for research. Volunteers receive $20 gift cards per household. State health officials will contact anyone whose results indicate an active infection.
The U.S. Centers for Disease Control and Prevention this summer estimated there are as many as 10 unknown infections for every known case. That suggests that roughly 800,000 Minnesotans have been infected, whether they know it or not — but subsequent prevalence studies around the country have failed to confirm that rate.
Commercial labs from 19 Minnesota counties and nine other U.S. regions are providing antibody testing results to the CDC. The prevalence rate has gradually increased in Minnesota, according to those results, from 2.2% in late May to 4.3% in June.
Diagnostic tests are based on genomic analysis of nasal or throat swab samples and determine if people are actively carrying the novel coronavirus that causes COVID-19. Seroprevalence antibody tests are based on blood serum and assess whether people's immune systems have reacted to the virus, indicating a prior infection.
The new research initiative comes as Minnesota health officials closely monitor daily COVID-19 activity reports and assess whether the resumption of K-12 and college classes have caused a new wave of cases.
Several indicators of pandemic severity are trending in the right direction, with the current positivity rate of diagnostic testing dipping below 5% and COVID-19 hospitalizations reaching a two-month low this week.
The state on Tuesday reported 238 COVID-19 hospitalizations, including 131 people in intensive care, along with five COVID-19 deaths and 432 coronavirus infections.
On the other hand, the 65 deaths reported since last Tuesday are the most in a seven-day period since late June.
Outbreaks of at least one case have been reported at 67 of Minnesota's 200 colleges and universities. The state has tallied 868 COVID-19 cases involving students or staff of colleges — though only 164 involved people living on campus at the time of their infections. Twenty-five colleges have five or more cases and three reported 100 or more in the past two weeks.
While seroprevalence studies can help tally the unknown and asymptomatic cases, they also have limits. Nobody yet knows how long antibodies remain and if they provide long-term protection from future infections.
"We're still learning information about whether that antibody response is fully protective and how long it lasts," said Stephanie Yendell, a senior epidemiology supervisor for the Health Department.
Some researchers nationally have reported cases of people who don't test positive for antibodies but show an immune system reaction to COVID-19 in their white blood T-cell counts. That could indicate a broader spread of the coronavirus than indicated by antibody test results as well.
Yendell said the new survey can get at that question by conducting antibody tests on people who previously tested positive for COVID-19. A high positive antibody rate in a county with a low COVID-19 case rate also suggests a lack of medical resources and the need to divert more testing opportunities, she said.
"A study like this is one of the best uses for antibody tests," she said. "It's helping us learn about a population, whereas its value is more limited [for] an individual — though certainly there is a lot of curiosity."
That curiosity prompted North Memorial Health last week to announce it was offering retail antibody testing for an out-of-pocket fee, following a similar announcement earlier in the summer by M Health Fairview.
Fairview had provided 2,538 retail COVID-19 antibody tests as of last week. Of those, 5.63% were positive.
Antibody test results aren't part of the state's COVID-19 case tally and don't contribute to county case rates that can be used to evaluate the safety of keeping schools open for in-person classes. Positive diagnostic tests in the study could inflate local community COVID-19 rates, but Yendell said the state testers are only spending a couple of days in any one location, so the impact should be minimal.
The random survey is modeled under the CDC's Community Assessment for Public Health Emergency Response, or CASPER, program. Similar surveys have amassed household information amid hurricanes, oil spills and the Zika virus outbreak. The Kauai health district in Hawaii used a CASPER survey to assess employment status and mental health amid the pandemic.
Yendell said aggregate results from the survey should be reported later this year. Individual results are kept private, and she added that people can volunteer for either or both tests.
Jeremy Olson • 612-673-7744

Marijuana's path to legality in Minnesota: A timeline
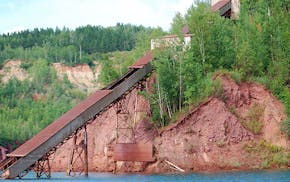
Minnesota to close state park on Iron Range, turn it back into a mine
U.S. Steel won't get exception to pollution rules that protect wild rice, MPCA says

Taste of Minnesota to be enjoyed on the ground and in the air this year

