Commentary
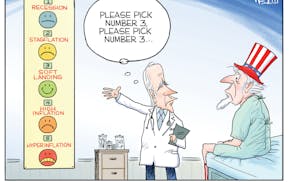
The recent cases of measles in Minneapolis vividly bring to light what many of us have long feared; that infant and childhood immunization rates are not at a level that will adequately protect our community from serious diseases that can easily be prevented.
Immunizations are a powerful public health tool, and we must do whatever we can to approach 100 percent vaccination.
Yet, our overall infant and childhood immunization rates are no better than 82 percent, and have stagnated there for several years.
The infections for which we have effective vaccines are serious, often associated with complications and even death.
It is unacceptable that children living in Minnesota in 2011 can die from a vaccine-preventable disease.
A number of factors contribute to lower immunization rates -- and each needs to be addressed head-on.
Persistent misinformation and misconceptions about immunizations threaten the health of all members of our society, but especially children.
For example, fears of an alleged link between the measles/mumps/rubella vaccine and autism, though the purported link has been soundly discredited, still persist in some communities, causing parents to opt out of the MMR vaccine.
We have seen the sad results with the spread of measles in our own communities.
The absence of major outbreaks of serious disease (such as polio) in recent decades has lulled many into thinking that vaccines are no longer needed, or that the perceived risk of side effects from vaccines is greater than the risk of the disease itself. Nothing could be further from the truth.
The absence of major disease outbreaks is evidence that vaccines work -- that our efforts to vaccinate children and others are paying off.
But we're not done yet. We must not let the absence of disease allow us to let down our guard.
These infections are still out there; some are endemic right here in Minnesota, and others are just a plane ride away.
Finally, some parents choose to delay certain vaccinations for their children out of a misguided fear of "overloading" their babies' immune systems.
The timetable for vaccination is carefully worked out by experts, basing the recommended vaccine schedule on when a child is most at risk for infections and yet at a time when their immune system can respond.
Exposure to the vaccine enables the development of an immune response so that when vaccinated children are exposed to an infectious agent, they can deal with the pathogen without getting sick and without spreading the infection.
Most healthy children have robust immune systems that can handle the small challenge posed by the vaccines. They are exposed to far greater amounts of pathogens in their everyday environments.
Given the persistence of misconceptions, it's clear that we need to improve and increase our educational efforts about the importance, safety and efficacy of vaccinations.
But what else can we do to raise immunization rates?
• For vaccine-hesitant parents, we can arm physicians and nurses with effective ways of addressing parents' concerns. On-the-fence parents want to discuss these issues with their doctors. Knowing what to say is only half of the battle; physicians need the time during a visit to have the conversation, and they need to be compensated for that time. Currently, administrative fees aren't necessarily covering the costs of this time.
• For uninsured and underinsured parents, we have the Minnesota Vaccine for Children (MnVFC) program, but parents may not be aware that they can get free shots, so they don't pursue preventive health care. We need to do better promotion of the program.
• We need to continue to address the social conditions that affect immunizations and other health issues: homelessness and dislocation of families, lack of access to health care and health insurance, and cultural barriers to understanding health information.
• We need to be sure that vaccination activities are part of health reform and that vaccination rates are used as one measure of the effectiveness of our reform efforts. The more we can do upstream with prevention, the less we will have to pay for downstream in health care.
Edward Ehlinger is commissioner of the Minnesota Department of Health.