Counterpoint
Few issues have become more politicized than health reform.
Even before the start of federal reform process, the rising cost of care was leveraged to advance agendas: from the government-run, single-payer system to the free-market system with minimal public involvement.
Much of the debate ignores the reality that health care costs are rising for many reasons. A person's health care spending spikes after age 55 -- and we are an aging population.
Thanks to technology, there are new treatments to treat conditions recently untreatable -- great news for the patient, expensive news for those paying for health care.
We don't take care of ourselves as well as we should.
These trends shouldn't be overlooked as state policymakers look to trim health costs as part of Minnesota's $5 billion budget shortfall. But good public policy can help manage costs.
That's the case Department of Human Services Commissioner Lucinda Jesson recently made in "A check-up for managed care" (Feb. 21).
She focused her attention on Minnesota's health plans and their role in public health programs, saying it is time for "a new model for delivery of high-quality, cost-effective care" and suggesting a study to assess managed care's value.
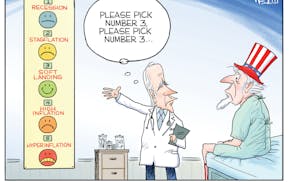
We embrace her recommendations and suggest that additional steps be taken to further control cost increases and make health care spending more transparent. Minnesota would be well-served by considering these three bold actions:
- Make transparency a reality, not just a goal.
Health plans are required to report an enormous amount of data. Anyone wanting to know the costs of public programs, including payments to health plans and their administrative overhead, can find it if they know how to navigate the system.
But it shouldn't be so hard. Currently, health plan information is sent to three state agencies -- health, commerce and human services.
The goal of transparency would be better served if all the data were made available on a single website and in a format that allowed for easy comparisons of actual costs.
In addition to the financial data for health plans, hospitals, clinics and others in the health care system, it would be good to build on Jesson's suggestion for a "report card" and provide details on how Minnesota and other states compare on costs and quality measures for plans, hospitals and providers.
Having a scorecard will help consumers and policymakers evaluate the data for themselves.
- Create more choices through effective competition in the health insurance marketplace.
Competition makes organizations stronger and energizes the marketplace. Creating a Minnesota insurance exchange will increase competition.
Through the exchange, consumers will be able to make side-by-side comparisons that lead to good choices. Current regulations should be evaluated to ensure they aren't hindering competition.
If the regulatory environment is level and all health insurers adhere to the same consumer protection rules, then Minnesota consumers will have good choices.
- Change how the state purchases health care coverage for poor Minnesotans.
For nearly 25 years, Minnesota HMOs have been required to cover individuals who qualify for state public programs. This mandate ensured that low-income people had access to health care when providers wouldn't serve them.
The state sets the rate it will pay the health plans, and the health plans are required to provide the coverage to any individual who qualifies. While this approach has provided access and value over time, there is interest in trying new innovations.
Payment reform and new models of care delivery, such as Accountable Care Organizations, should be on the table. Minnesota should also examine what other states are doing.
There are many models at work, and it is time to consider different approaches that preserve choice for the individuals and families served.
Everyone agrees: The state needs to be a smart purchaser of health care, and the current system needs to improve. During these times, Minnesota's health plans are ready not just to be part of the health care solution, but to make them a reality.
Julie Brunner is executive director of the Minnesota Council of Health Plans.
* * *
Readers, what do you think? To offer an opinion considered for publication as a letter to the editor, write no more than 250 words to opinion@startribune.com. Include your name and the city where you live.
Follow us on Twitter @StribOpinion