There are rumblings that the glitches attending the rollout of the Affordable Care Act - along with the relentless campaign to sabotage or delay it in numerous states - mean the program is dead on arrival. But the history of an equally controversial and vast government effort, Medicare, indicates that predictions of Obamacare's demise are greatly exaggerated.
Medicare became law July 30, 1965, after a decades-long legislative struggle to create government-sponsored health care for all Americans 65 and older. Like the Affordable Health Care Act, Medicare required that people register for it. Then, as now, problems immediately surfaced, threatening to imperil the program.
For starters, few in the government seem to have realized that more than 45 percent of those born between 1890 and 1920 couldn't prove their age because they lacked birth certificates. While the government accepted other documentation such as military records or naturalization records, some pretty unorthodox records ended up being used. The New York Times reported that in one case, a man "bared his chest as a last resort. Tattooed there was the date of his enlistment in the Navy and the date of his birth." Another applicant dug up his mother's tombstone and carted into the local office, arguing that it constituted proof of his age. This, too, was accepted.
In the fall of 1965, millions started to enroll, no doubt aided by the reasonable ease of proving one's age. But ignorance of how the law actually worked became a serious problem by that time. More than 700,000 of those eligible for supplemental coverage refused to sign up in the opening months. Despite an elaborate public-relations campaign featuring celebrities such as Jimmy Durante and Bob Hope, and a door-to-door effort by canvassers who sought out the elderly at home, many older people believed that signing up for Medicare meant they would cease receiving Social Security. Others thought they couldn't afford the $3 monthly premium, even though the law had provisions to assist low-income enrollees.
As the date for Medicare's formal beginning approached, more serious problems cropped up. The most serious was a campaign by many doctors to boycott the program. In the months leading up to the final legislative debates, and after, the American Medical Association faced a revolt in its ranks over the issue, though it reluctantly endorsed cooperation. The Association of American Physicians and Surgeons, organized to combat "socialized medicine," came out against the law, urging "nonparticipation." The organization predicted that 50,000 doctors nationwide would refuse to play ball.
Most doctors didn't end up boycotting Medicare. The real threat came from elsewhere. Because Medicare involved federal aid to the states, participating institutions had to comply with Title VI of the Civil Rights Act of 1964, which banned racial discrimination. Hospitals in the South, which segregated patients by race, initially refused to comply with the law. As conflicts between hospital administrators and the federal government intensified, the president of the Louisiana Hospital Association put the matter bluntly: "It's the requirement that Negroes and whites be permitted to share the same hospital room," he warned. "I don't know what the hospitals will do but I hear that some of them don't see how they can comply."
Some hospitals didn't: when Medicare began on July 1, 1966, large swaths of the hospital system in the South remained segregated. Despite appeals by President Lyndon Johnson on television and radio, three-fourths of the hospitals in Mississippi couldn't accept Medicare patients when the program went into effect. Entire cities in the region - Selma, Ala., and Macon, Ga. - had no hospitals eligible for Medicare.
During the summer of 1966, more problems had piled up. Although predictions that hospitals would be overrun with elderly patients on July 1 proved unfounded, a key portion of the Medicare program - nursing home care - had yet to go into effect. Nor had the program weathered the more difficult winter months, when many elderly came down with infectious diseases.
Predictions of doom soon filled the nation's papers, with eminent voices from both sides of the political spectrum warning of the coming disaster. Sen. Edward Kennedy ominously predicted that the nation would need a half-million more nursing home beds; the Wall Street Journal warned of a "patient pileup" at hospitals. Hospital administrators grumbled, complaining of delays processing patients, overcrowding, and a host of related ills.
In the end, the nation's health-care system weathered these crises, even as new ones materialized. Under Medicare, doctors could either bill participating insurance providers or patients, who would then need to submit receipts for reimbursement. In the first years of the program, the majority of doctors billed their patients. When these patients - many of them on fixed incomes, with little cushion of savings - submitted their bills, it took them an average of two months to receive reimbursement. Stories of much longer waits became commonplace in the media.
Eventually, the government and the private insurers worked out most of the kinks, and by the late 1960s the system was working reasonably well. Almost all hospitals had desegregated, doctors dropped their opposition and claims processing improved.
It was far from perfect. Fraudulent claims became a growing problem, as did increasingly burdensome paperwork for doctors. But in general, the program worked as planned, even if it was less efficient, more expensive and a bit more troubled than its most enthusiastic boosters predicted.
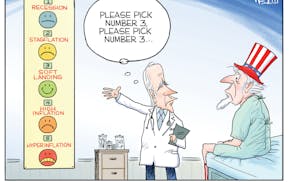
Similarly, Obamacare is probably here to stay. But judging from the history of Medicare's missteps, the new health insurance program will spend much more time in intensive care than anyone imagined.
Stephen Mihm is an associate professor of history at the University of Georgia.
Lab-grown beef is red meat for the conservative base