The last thing a cancer patient should have to worry about is whether lifesaving drugs administered at a hospital are real or counterfeit.
While an individual's chance of getting fake medications is small, the unfortunate truth is that the risk is real and that the United States is underequipped to combat what experts agree is an emerging public health threat: drugs whose potency is compromised by theft or fraudulent wholesalers and manufacturers.
Just last month came confirmation that counterfeit doses of the critical cancer drug Avastin have been distributed in the United States. Authorities also aren't able to account for most of the 129,000 vials of insulin stolen in 2009 when thieves drove off with a truckload of this crucial diabetes treatment, which needs to be refrigerated. They do know that some of the insulin went through licensed wholesalers in at least two states and into retail drug stores.
"The United States lacks strong, uniform national standards for licensure of pharmaceutical wholesalers, and we lack a standard system for companies to keep track of our pharmaceuticals during distribution," said Allan Coukell, the Pew Health Group's medical director, at a March 8 congressional hearing. "There is currently no way to check whether an individual vial or bottle is authentic or counterfeit."
While there's movement in some states, including Minnesota, to review or improve safeguards, national measures are the swiftest way to protect consumers. It's also in the industry's best interest to have one set of requirements rather than a state-by-state patchwork of rules.
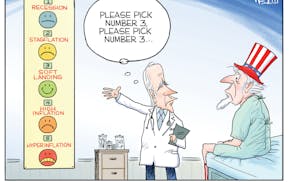
Congress is currently weighing proposals to strengthen federal wholesaler licensing requirements, which would help prevent stolen or fake drugs from entering the supply chain. There are also timely calls for a nationwide system to readily "track and trace" drugs through the distribution process.
In an era where bar-coding technology is widespread, consumers might think a system exists already to quickly authenticate drugs at each step of the process and pinpoint pharmacies or other settings where compromised medications have wound up. It does not.
Instead, the current system's tracking inadequacies mirror tracing problems that surfaced during a salmonella outbreak linked to peanut butter in 2009. Once the product left its Georgia processing plant, authorities could only slowly and incompletely piece together its distribution as it was used by other manufacturers or made its way to stores. The delay put consumers unnecessarily at risk.
Congress is weighing various drug "track and trace" proposals. Lawmakers should embrace the strongest possible system, which would put a unique serial number on each bottle or vial, and have distributors, pharmacists and other staff scanning the number as it moves through the distribution process. Counterfeiters could try to replicate bar codes, but multiple verification scans could catch fake or repetitive codes.
There would be cost associated with the bar-code equipment and staff time needed to scan. But industry, which has generally supported a weaker track-and-trace system, has a business interest in being able to quickly announce where compromised drugs are and who has them. More importantly, doing so will save lives.
"It's absolutely necessary to have a national tracking system in place," said Cody Wiberg, executive director of the Minnesota Board of Pharmacy. "It should have been done a long time ago, in my opinion."
----------
Readers, what do you think? To offer an opinion considered for publication as a letter to the editor, please fill out this form. Follow us on Twitter @StribOpinion and Facebook at facebook.com/StribOpinion.
Lab-grown beef is red meat for the conservative base