Minnesota has failed to properly vet people enrolling in a $550 million taxpayer-subsidized health insurance program despite a decade of warnings that it was breaking state and federal law, according to the Legislative Auditor.
The Department of Human Services (DHS) has known for years it was failing to properly verify the income and Social Security numbers of applicants for MinnesotaCare, Legislative Auditor Jim Nobles said in a report issued Tuesday. MinnesotaCare, created to insure people who can't afford private health insurance but don't qualify for Medicaid, covers about 129,000 people.
Nobles said income and eligibility verification are critical in publicly funded programs to reduce the risk of fraud and mistakes.
"This is not just a nice thing to do," Nobles said. "It's a requirement of both state and federal law. The department has not been in compliance with the law."
Human Services Commissioner Lucinda Jesson, in a letter to Nobles, agreed with the findings and said her agency takes the issues "very seriously."
"We will work diligently to correct them," Jesson said.
Human Services officials say a computer system that will be launched this year as part of Minnesota's health insurance exchange, known as MNsure, should fix the problem, but Nobles said he remains skeptical. After his office issued a report in 2003 identifying the eligibility problem, DHS said it was developing a new Web-based system to fix the issue. Years later, after spending $40 million, the agency scrapped that effort with no fix.
"It was a complete failure," Nobles said. "It was abandoned. Now we say the computer fix is going to be in the development of the insurance exchange. I certainly hope that will be true. But it isn't going to happen by magic."
Rep. Jim Abeler, R-Anoka, a health policy leader in the Republican caucus, said Minnesota has long operated a pay-first, verify-later approach to its public assistance programs. For years, legislators have received anecdotal reports of fraud or mistakes within the system, but state policies have not done enough to catch them.
"We're far too trusting," Abeler said. "In times when we are running a lean budget, that means people who are not entitled to things are getting things that they shouldn't have gotten."
Chuck Johnson, DHS chief financial and operating officer, said the agency conducts some forms of income verification, just not enough to meet federal requirements. That will change in January, when the new health exchange program loops into federal databases to allow for additional checks as part of the federal health overhaul.
"That will put us on a path to be back in compliance," Johnson said.
Brad Schrade • 612-673-4777
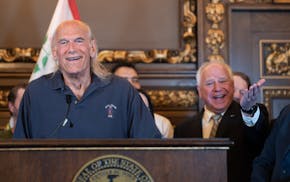
Former Gov. Jesse Ventura boasts he could beat unpopular Trump or Biden if he ran for president

Dave Kleis says he won't run for sixth term as St. Cloud mayor
Newspaper boxes repurposed as 'Save a Life' naloxone dispensaries

St. Cloud house vies for Ugliest House in America

